Johns Hopkins researchers have developed a revolutionary and reproducible new model material that not only looks and feels like human skin but also mimics its complex system of capillaries, the body’s smallest and most numerous blood vessels. This novel skin “phantom” promises to help researchers develop new non-invasive technologies to monitor and detect diseases and enable them to study the various chemical compounds that move through and beneath layers of skin.
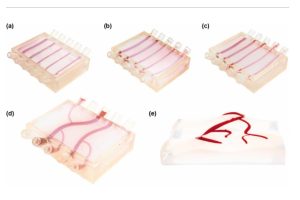
Led by Ishan Barman, a professor of mechanical engineering at the Whiting School of Engineering, the team created this 3D network of mini-fluidic channels specifically to further research into metabolic function using Raman spectroscopy—a technique that uses electromagnetic light readings from lasers to detect diseases within the body.
“Together with advances in Raman spectroscopy, these new phantoms are bringing the ‘holy grail’ that will allow us to non-invasively analyze and monitor analyte—the chemical constituents—of blood closer and closer,” Barman said. “That has been a basic goal of optical technologies used in the biomedical domain for a long time.”
The team’s research appeared in Sensors and Actuators B: Chemical.
The breakthrough is the team’s success in recreating the internal highway of blood within layers of the skin prototype, which Barman said has long been a challenge.
“There are other vascular phantoms or organoids that have been created, but none specifically to further develop Raman spectroscopy as a non-invasive technique,” Piyush Raj, a graduate student in the Barman laboratory and one of the paper’s lead authors, said. “It’s really hard to mimic vasculature, and for the most part, it’s not been done at this scale. We are most interested in mimicking the capillaries, most of which are in the millimeter scale.”
This could allow monitoring of diseases such as diabetes without the painful finger prick, for example.
“Imagine being able to monitor glucose in the bloodstream using minimally invasive sensors,” Barman said. “That’s the goal.”
Lintong Wu, another lead author of the paper, said that monitoring analytes through the skin is particularly challenging because it is subject to outside influences such as sweat, neighboring cell clusters, hydration level, and even the amount of melanin, all of which can skew or obscure results or diagnosis. Bones can get in the way, too, causing a scattering effect.
“A lot of studies have failed to capture that,” Barman said. “And that is why their model works for a short period, and soon after starts giving errors in the results.”

Ishan Barman
By training Raman spectroscopy on the team’s phantom, researchers can fine-tune the process to account for such inaccuracies.
“We built this with the idea that it has some tunability, and we are introducing more programmability into the next-gen,” Barman said.
Down the road, Barman envisions instant monitoring of metabolite activity via surface skin readings.
“We have Apple Watches and Fitbits and wearables, etc., which are monitoring our heart rates and so on,” he said. “It would be cool if you could actually use that to monitor more complex biomarkers for different pathological conditions.”
Hopkins PhD student Saransh Arora in the Department of Mechanical Engineering and Assistant Professor Luo Gu and PhD students Zhiwei Fang and Yi Zuo from the Department of Materials Science and Engineering contributed to this research.
Interview conducted by Roberto Molar Candanosa.