Removal of cancerous tumors, or resection, in delicate areas like the head and neck is a challenge for even the most experienced surgeons. When removing cancerous tissue, the aim is to preserve as much healthy tissue as possible to prevent unnecessary losses to the patient; however, removing too little tissue risks leaving behind cancer cells that may return or even spread. Factored into this delicate equation are inherent mental and physical obstacles like fatigue, burnout, and visual obstruction, which the steadiest of hands and the best of intentions cannot always overcome.
Enter ASTR: the Autonomous System for Tumor Resection. Designed by a team of Johns Hopkins researchers to overcome those human factors, ASTR can remove tumors from the tongue with accuracy rivaling—or even potentially exceeding—that of human surgeons.
The team’s research, “Autonomous System for Tumor Resection (ASTR) – Dual-Arm Robotic Midline Partial Glossectomy” appeared in Institute of Electrical and Electronics Engineers Robotic and Automation Letters.
“Doing a resection that has precise margins is a super difficult task,” said team leader Axel Krieger, assistant professor of mechanical engineering at the Whiting School of Engineering. “So much of these surgeries is hope and even some guessing. A lot of surgeons struggle with it. Our goal was to make these procedures more precise.”
Precise in this case is 5mm of healthy tissue—the standard surgeons aim for when removing cancerous tissue. That 5mm—about the size of an eraser at the end of a pencil—is enough to ensure that the affected cells are included while keeping the overall damage minimal. Complicating things is the fact that cancerous tumors can often present as having visible horizontal borders on the edges, but less obvious vertical borders.

Axel Krieger
“The problem we heard from many of the surgeons we collaborate with is that it’s so hard to resection a tumor precisely,” Krieger said. “Surgeons bring a little ruler in and see the 5mm distance and mark off the edges on the sides. But how deep to go—that’s so difficult.”
Doctoral student and team member Jiawei Ge said that even though pre-surgery preparation is painstakingly thorough, that crucial 5mm border acts as a blind zone.
“The challenge is that surgeons do not have direct access to the tumor, due to surrounding tissue,” Ge said. “They can see the surface of the tumor, but otherwise can only see the healthy tissue. The map is in the surgeon’s mind.”
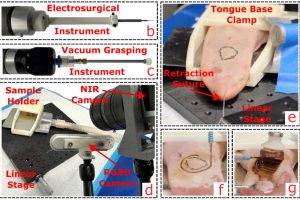
ASTR works by translating human guidance into robotic precision. Using porcine tongue tissue, the team drew outlines of tumors based on empirical research and programmed ASTR to remove the tumor and exactly 5mm of healthy tissue using its combination of vacuum grasping and cutting. ASTR succeeded each time and did not require stoppage by the supervisors.
“The physician can supervise the robot and give pre-surgery inputs, then the robot does it step by step,” Krieger said. “What we showed is that surgeons can get very good horizontal margins with the ruler, but on the depth margins our robot really shows improvement.”
Krieger and his team based their new robotic system on technology they developed for their Smart Tissue Autonomous Robot (STAR), which made international news two years ago for performing the first fully autonomous laparoscopic surgery: a procedure to connect two ends of an intestine. The researchers adapted STAR’s technical workings to create ASTR’s new, autonomous, dual-arm, vision-guided robotic system. But while STAR focused on connecting tissue, ASTR is specifically tailored to remove it.
“We’ve sent the robot to make an incision before, but this is the first time we’ve done a bulk resection and taken a tumor out fully,” Krieger said. “That’s the big novelty here.”
Tumors of the tongue, the removal of which is called a partial glossectomy, presented what Krieger called an ideal case due to their surface accessibility and current use in experimental surgery. Cancer of the tongue, while rare, has stricken celebrities Michael Douglas and Eddie Van Halen. In the latter case, initial surgeries were unsuccessful and required further resection, but the ensuing metastasis claimed the musician’s life.
Krieger said that the next step is internal organs like the kidney, which require internal surgery and dissection to access the tumor. Pairing ASTR’s precision surgery with precision imaging could be the ultimate game-changer in tumor resection treatment.
“They use robots a lot already in clinical practice, so this isn’t a huge paradigm shift,” Krieger said.